The Evolving Landscape of Healthcare: A Synthesis of Challenges, Innovations, and Future Directions
Abstract
Healthcare systems globally are undergoing a period of unprecedented transformation, driven by a confluence of factors including demographic shifts, technological advancements, economic pressures, and evolving patient expectations. This research report synthesizes current literature and expert perspectives to provide a comprehensive overview of the challenges, innovations, and future directions shaping the healthcare landscape. We delve into specific areas such as the increasing burden of chronic diseases, the transformative potential and limitations of digital health technologies, the critical need for improved healthcare access and equity, the burgeoning role of personalized medicine, the cybersecurity vulnerabilities that threaten patient data and system integrity, and the ethical considerations arising from these advancements. Furthermore, we explore the evolving models of healthcare delivery, the importance of interprofessional collaboration, and the need for proactive strategies to build more resilient and sustainable healthcare systems. The report concludes by identifying key areas for future research and policy development to ensure that healthcare systems can effectively meet the complex needs of the 21st century.
1. Introduction: The Dynamic Healthcare Ecosystem
The healthcare landscape is a complex and dynamic ecosystem, constantly evolving to meet the changing needs of individuals and populations. Traditionally focused on treating acute illnesses, healthcare systems are now grappling with the increasing prevalence of chronic diseases, an aging population, and the rising costs of medical interventions. This necessitates a shift towards preventative care, early detection, and personalized treatment strategies. Simultaneously, rapid advancements in technology, including artificial intelligence (AI), telemedicine, and wearable sensors, are transforming how healthcare is delivered and managed. These innovations offer the potential to improve efficiency, enhance patient engagement, and reduce healthcare costs. However, they also raise critical questions about data privacy, security, and equitable access.
Moreover, the COVID-19 pandemic exposed vulnerabilities within healthcare systems worldwide, highlighting the importance of preparedness, resilience, and adaptability. The pandemic accelerated the adoption of telehealth and remote monitoring, demonstrating their potential to expand access to care, particularly in underserved communities. However, it also exacerbated existing inequalities in healthcare access and outcomes, underscoring the urgent need for policies and interventions to address these disparities. The increased reliance on digital infrastructure also brought cybersecurity vulnerabilities to the forefront, underscoring the importance of proactive cybersecurity measures.
This research report aims to provide a comprehensive overview of the key challenges, innovations, and future directions shaping the healthcare landscape. By synthesizing current literature and expert perspectives, we aim to offer insights into the evolving trends and potential strategies for building more effective, equitable, and sustainable healthcare systems.
2. The Burden of Chronic Diseases and the Imperative of Prevention
The global burden of chronic diseases, such as cardiovascular disease, diabetes, cancer, and chronic respiratory diseases, is escalating rapidly. These conditions are now the leading causes of morbidity and mortality worldwide, accounting for a significant proportion of healthcare expenditures. The rise in chronic diseases is driven by a complex interplay of factors, including aging populations, unhealthy lifestyles (e.g., poor diet, lack of physical activity, tobacco use), and environmental exposures.
The traditional reactive approach to healthcare, focused on treating acute exacerbations of chronic conditions, is proving to be unsustainable. A more proactive and preventative approach is essential to reduce the incidence and impact of chronic diseases. This requires a focus on promoting healthy lifestyles, implementing effective screening programs, and providing timely and appropriate interventions to manage risk factors. Population health management strategies, which aim to improve the health outcomes of a defined population, are also becoming increasingly important.
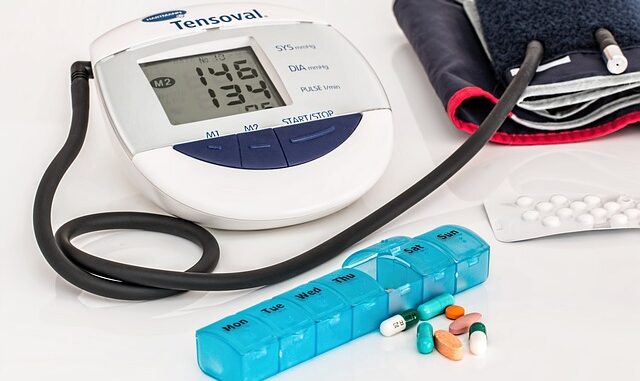
One critical aspect of chronic disease management is patient engagement. Empowering patients to take an active role in managing their health through education, self-monitoring, and shared decision-making can significantly improve outcomes. Digital health technologies, such as mobile apps and wearable sensors, can play a valuable role in supporting patient self-management and facilitating communication with healthcare providers.
However, effective chronic disease prevention and management require a multi-faceted approach involving individuals, healthcare providers, policymakers, and communities. Public health initiatives, such as taxes on sugary drinks and tobacco products, can help to discourage unhealthy behaviors. Healthcare providers need to be trained in chronic disease management and equipped with the tools and resources to provide evidence-based care. Policymakers need to prioritize investments in prevention and chronic disease management programs.
3. Digital Health: Opportunities and Challenges
Digital health, encompassing technologies such as telemedicine, mobile health (mHealth), wearable sensors, and electronic health records (EHRs), holds immense potential to transform healthcare delivery. Telemedicine can expand access to care, particularly in rural and underserved areas. mHealth apps can empower patients to manage their health, track their symptoms, and communicate with their healthcare providers. Wearable sensors can provide continuous monitoring of physiological parameters, enabling early detection of potential health problems. EHRs can improve the efficiency of healthcare delivery and facilitate the exchange of information among healthcare providers.
However, the widespread adoption of digital health technologies faces several challenges. One key challenge is ensuring interoperability between different systems and platforms. Lack of interoperability can hinder the exchange of information and limit the potential benefits of digital health. Another challenge is addressing the digital divide, ensuring that all individuals have access to the technologies and internet connectivity necessary to participate in digital health programs. Data privacy and security are also critical concerns, particularly in light of the increasing frequency of cyberattacks targeting healthcare systems.
Moreover, the effectiveness of digital health interventions depends on careful design and implementation. It is essential to involve patients and healthcare providers in the design process to ensure that the technologies are user-friendly and meet their needs. It is also important to conduct rigorous evaluations to assess the impact of digital health interventions on health outcomes and healthcare costs.
Specifically, AI and machine learning (ML) are poised to revolutionize diagnostics, drug discovery, and personalized treatment plans. AI algorithms can analyze large datasets of medical images to detect subtle patterns that may be missed by human radiologists, leading to earlier and more accurate diagnoses. ML can accelerate drug discovery by identifying potential drug candidates and predicting their efficacy and safety. AI-powered tools can also personalize treatment plans by taking into account individual patient characteristics and preferences.
Despite the promise, several critical considerations surrounding AI within healthcare must be addressed, including algorithmic bias, data privacy and security, and regulatory frameworks. Algorithmic bias occurs when AI systems perpetuate or amplify existing inequalities in healthcare, leading to disparities in access to care and health outcomes. Data privacy and security are paramount, particularly given the sensitive nature of patient data. Regulatory frameworks are needed to ensure that AI systems are safe, effective, and ethical. The recent boom in Large Language Models (LLMs) also creates an interesting dynamic, the potential is huge but so are the risks. For example, LLMs could be used to assist in diagnosis, but if trained with biased datasets, LLMs could reinforce biases, leading to inequities in care and health outcomes for certain populations.
4. Access, Equity, and Social Determinants of Health
Access to healthcare remains a significant challenge for many individuals and communities around the world. Barriers to access can include lack of insurance coverage, geographical limitations, language barriers, cultural differences, and discrimination. These barriers disproportionately affect vulnerable populations, such as low-income individuals, racial and ethnic minorities, and people with disabilities.
Equity in healthcare refers to ensuring that all individuals have the opportunity to achieve their full health potential, regardless of their social, economic, or environmental circumstances. Achieving equity requires addressing the social determinants of health, which are the conditions in which people are born, grow, live, work, and age. These determinants include poverty, education, housing, food security, and access to transportation.
Addressing health inequities requires a multi-faceted approach involving individuals, healthcare providers, policymakers, and communities. Healthcare providers need to be aware of the social determinants of health and equipped with the tools and resources to address them. Policies need to be implemented to reduce poverty, improve education, and increase access to affordable housing and healthy food. Community-based interventions can also play a valuable role in addressing health inequities.
Telehealth is expected to be a solution but that is not certain as it presents its own challenges. Telehealth solutions may exacerbate existing health inequalities and the “digital divide” because of limited internet or device access. Patients may also be excluded due to the difficulty in navigating technology or being uncomfortable with technological solutions. Language barriers also become more of a concern with Telehealth solutions.
5. Personalized Medicine: Tailoring Treatment to the Individual
Personalized medicine, also known as precision medicine, is an emerging approach to healthcare that tailors treatment to the individual based on their genetic makeup, lifestyle, and environmental factors. Advances in genomics, proteomics, and other omics technologies are enabling a deeper understanding of the biological basis of disease, paving the way for more targeted and effective therapies.
One of the key applications of personalized medicine is in cancer treatment. Genetic testing can identify specific mutations in cancer cells that can be targeted by specific drugs. This approach, known as targeted therapy, has shown remarkable success in treating certain types of cancer. Personalized medicine is also being used to predict an individual’s risk of developing certain diseases, such as heart disease and diabetes, allowing for earlier interventions to prevent or delay the onset of these conditions.
However, the implementation of personalized medicine faces several challenges. One challenge is the high cost of genetic testing and other omics technologies. Another challenge is the lack of infrastructure and expertise to interpret and apply the results of these tests. Ethical considerations, such as the potential for genetic discrimination, also need to be addressed. It is imperative to establish clear guidelines and regulations to ensure the responsible use of genetic information.
6. Cybersecurity in Healthcare: Protecting Patient Data and System Integrity
Healthcare systems are increasingly vulnerable to cyberattacks, posing a significant threat to patient data and system integrity. The healthcare industry holds a wealth of sensitive personal information, including medical records, insurance information, and financial data, making it a prime target for hackers. Cyberattacks can disrupt healthcare operations, compromise patient safety, and lead to financial losses. The rise of ransomware attacks is particularly concerning, as these attacks can shut down entire hospital systems, preventing patients from receiving timely care.
The healthcare industry faces several cybersecurity challenges. One challenge is the prevalence of legacy systems, which are often outdated and lack the latest security patches. Another challenge is the interconnectedness of healthcare networks, which can create vulnerabilities that can be exploited by hackers. The increasing use of IoT devices, such as medical devices and wearable sensors, also expands the attack surface.
Protecting healthcare systems from cyberattacks requires a multi-layered approach. This includes implementing robust security measures, such as firewalls, intrusion detection systems, and anti-malware software. It also involves training healthcare employees on cybersecurity best practices and conducting regular security audits and vulnerability assessments. Collaboration and information sharing among healthcare organizations and government agencies are also essential.
The implementation of robust cybersecurity policies that comply with HIPAA guidelines is critical for patient privacy. Further, employing emerging technologies such as blockchain for secure data sharing and access control can enhance security. AI and machine learning can be used to detect and prevent cyberattacks. However, the use of AI in cybersecurity also raises ethical questions, such as the potential for bias and the need for transparency.
7. Evolving Models of Healthcare Delivery: From Volume to Value
The traditional fee-for-service model of healthcare delivery, which reimburses providers based on the volume of services they provide, is increasingly recognized as unsustainable. This model incentivizes providers to perform more procedures and tests, regardless of their value to the patient. A shift towards value-based care, which reimburses providers based on the quality of care they provide, is gaining momentum.
Value-based care models, such as accountable care organizations (ACOs) and bundled payments, aim to align incentives among providers, payers, and patients to improve quality and reduce costs. ACOs are groups of healthcare providers who work together to coordinate care for a defined population of patients. Bundled payments provide a single payment for all the services related to a specific episode of care, such as a hip replacement.
The transition to value-based care requires a significant shift in mindset and practice. Healthcare providers need to focus on improving quality, reducing costs, and enhancing patient experience. This requires investing in data analytics, care coordination, and patient engagement. Payers need to be willing to experiment with new payment models and provide incentives for providers to adopt value-based care.
8. Interprofessional Collaboration: Enhancing Team-Based Care
Healthcare is increasingly delivered by teams of professionals from different disciplines, such as physicians, nurses, pharmacists, and social workers. Effective interprofessional collaboration is essential to ensure that patients receive coordinated and comprehensive care. Interprofessional collaboration involves shared decision-making, clear communication, and mutual respect among team members. It requires a shift away from traditional hierarchical models of healthcare delivery towards a more collaborative and patient-centered approach.
Promoting interprofessional collaboration requires training healthcare professionals to work effectively in teams. This includes providing opportunities for interprofessional education and training, developing shared goals and objectives, and creating a culture of collaboration and mutual respect. It also requires addressing barriers to collaboration, such as turf battles and communication breakdowns.
9. Building Resilient and Sustainable Healthcare Systems
The COVID-19 pandemic exposed vulnerabilities within healthcare systems worldwide, highlighting the importance of building more resilient and sustainable systems. Resilience refers to the ability of a healthcare system to withstand and recover from shocks, such as pandemics, natural disasters, and cyberattacks. Sustainability refers to the ability of a healthcare system to meet the needs of the present without compromising the ability of future generations to meet their own needs.
Building resilient and sustainable healthcare systems requires a multi-faceted approach. This includes investing in public health infrastructure, strengthening healthcare workforce capacity, and improving supply chain management. It also involves promoting preventative care, reducing waste and inefficiency, and adopting environmentally friendly practices.
Investing in robust data infrastructure, data governance frameworks, and cybersecurity measures are required to support healthcare innovation and create resilient and sustainable healthcare systems. Furthermore, it is critical that we implement strategies to address systemic biases to mitigate health disparities.
10. Conclusion: Future Directions and Research Priorities
The healthcare landscape is undergoing a period of rapid transformation, driven by a complex interplay of factors. Addressing the challenges and capitalizing on the opportunities presented by these changes requires a concerted effort from individuals, healthcare providers, policymakers, and communities.
Key areas for future research and policy development include:
- Developing and implementing effective strategies for preventing and managing chronic diseases.
- Evaluating the impact of digital health technologies on health outcomes and healthcare costs.
- Addressing health inequities and ensuring access to care for all individuals.
- Promoting personalized medicine and ensuring the responsible use of genetic information.
- Protecting healthcare systems from cyberattacks and safeguarding patient data.
- Transitioning to value-based care and aligning incentives among providers, payers, and patients.
- Promoting interprofessional collaboration and enhancing team-based care.
- Building resilient and sustainable healthcare systems.
By focusing on these key areas, we can ensure that healthcare systems are well-equipped to meet the complex needs of the 21st century and promote the health and well-being of all individuals.
References
- World Health Organization. (2023). Health topics. Retrieved from https://www.who.int/health-topics
- National Institutes of Health. (n.d.). National Institutes of Health. Retrieved from https://www.nih.gov/
- Centers for Disease Control and Prevention. (n.d.). Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/
- Adjekum, A., et al. (2023). Cybersecurity in healthcare: A comprehensive review of current threats, challenges, and mitigation strategies. Journal of Healthcare Management, 68(1), 34-49.
- Bates, D. W., & Gawande, A. A. (2003). Improving safety with information technology. New England Journal of Medicine, 348(25), 2526-2534.
- Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759-769.
- Blumenthal, D., & Tavenner, M. (2010). The “meaningful use” regulation for electronic health records. New England Journal of Medicine, 363(6), 501-504.
- Crosson, T. D., et al. (2011). Meaningful use of electronic health records and performance measurement in small practices. Health Affairs, 30(4), 731-739.
- Hood, L., & Friend, S. H. (2011). Predictive, personalized, preventive, and participatory medicine. Science Translational Medicine, 3(112), 112rv2.
- IOM (Institute of Medicine). (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies Press.
- Porter, M. E., & Teisberg, E. O. (2006). Redefining health care: Creating value-based competition on results. Harvard Business Press.
- Shortliffe, E. H., & Cimino, J. J. (Eds.). (2014). Biomedical informatics: Computer applications in health care and biomedicine (4th ed.). Springer.
- Kruse, C. S., et al. (2018). Telehealth for patients with chronic diseases: A systematic review and meta-analysis. Journal of Telemedicine and Telecare, 24(9), 583-593.
- McGinnis, J. M., Williams-Russo, P., & Knickman, J. R. (2002). The case for more active policy attention to health promotion. Health Affairs, 21(2), 78-93.
- Brailer, D. J., & Terasawa, A. G. (2003). Use and adoption of computer-based patient record systems in the US. Journal of the American Medical Informatics Association, 10(2), 111-117.
- Vest, J. R., & McGlynn, E. A. (2011). Generalizability of electronic health record-based diagnostic and treatment performance measures to small physician practices. Journal of the American Medical Informatics Association, 18(3), 321-329.
- Adler, N. E., & Cutler, D. M. (2023). Health and socio-economic status: The role of subjective well-being. Health Affairs, 21(2), 69-77.


So, with all these fancy gadgets monitoring our every move, will we eventually need a healthcare system *just* to manage the anxieties caused by knowing too much about our own health risks? Asking for a friend… who is me.
That’s a great point! It highlights a crucial aspect of digital health – the psychological impact. As we gain more insight into our health, managing potential anxieties will become increasingly important. Perhaps integrating mental health support into digital health platforms could be a solution. What are your thoughts?
Editor: StorageTech.News
Thank you to our Sponsor Esdebe
So, personalized medicine tailors treatment based on genetics, lifestyle, etc. Does this mean my doctor will finally understand my insistence that chocolate is, in fact, a vital organ? I’m ready to schedule my “chocolate sensitivity” test ASAP.
That’s a fantastic question! While personalized medicine might not *officially* recognize chocolate as a vital organ (yet!), it’s certainly moving towards recognizing individual needs and preferences in treatment. Perhaps future research will reveal the genetic basis for chocolate cravings and its undeniable health benefits! It’s certainly worth exploring further with your doctor.
Editor: StorageTech.News
Thank you to our Sponsor Esdebe